Hormones play an intricate role in the orchestra of male reproductive health, with key players such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), and testosterone acting as the principal conductors of fertility. Imbalances in these hormones can lead to marked changes in sperm production and overall fertility, while a skewed ratio of estrogen to testosterone, abnormal levels of prolactin, or thyroid-stimulating hormone (TSH) can also exert significant influence. Indicators of such hormonal imbalance may manifest as diverse symptoms, indicating disturbances in the delicate endocrine system that are central to male fertility.
Recognizing the criticality of hormonal balance, this article aims to unravel the complexities of male hormones and their profound impact on fertility, including the underlying conditions that may lead to hormonal imbalance such as varicocele, erectile dysfunction, and other reproductive health concerns. Testing and regulation of hormones like FSH, LH, and testosterone are essential for maintaining reproductive health and addressing infertility. The forthcoming sections will discuss the symptoms of hormonal imbalance in men, factors contributing to these irregularities, strategies to harmonize hormonal levels, and the necessity of medical consultation to manage and optimize sperm count and fertility.
Understanding Hormones in Male Reproductive Health
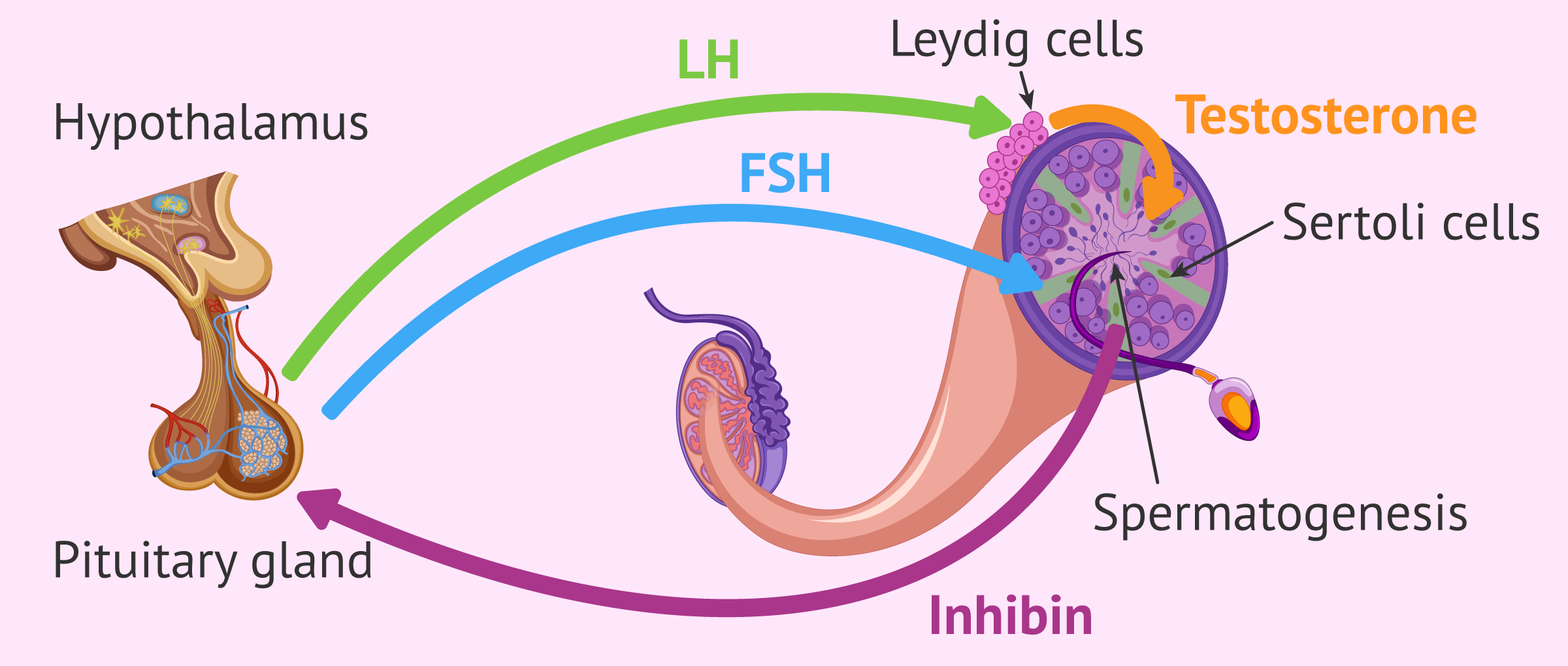
Hormones are the unsung heroes of the male reproductive system, functioning as chemical messengers that regulate a myriad of processes essential for fertility. They are responsible for controlling muscle mass, emotions, and most notably, sex drive. The Hypothalamic-pituitary Gonadal Axis (HPG) is a communication network comprising the hypothalamus, pituitary gland, and testes, which is pivotal in the development and regulation of the reproductive and immune systems.
The Hypothalamic-Pituitary Gonadal Axis (HPG):
- Hypothalamus Function: Releases Gonadotropin-Releasing Hormone (GnRH).
- Pituitary Gland Response: Produces Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH) upon stimulation by GnRH.
- Testes Activation: FSH and LH stimulate the testes to produce androgens (like testosterone) and sperm.
Testosterone, which is synthesized by Leydig cells in the testes, is indispensable for normal growth and development in men. It contributes to the development of body and facial hair, functions of the larynx, genital enlargement, and secondary sex characteristics.
Testosterone’s Role in Sperm Production:
- Sperm Production: Testosterone works alongside FSH to stimulate the production of sperm.
- Sexual Function: Regulates the flow of sperm during sexual intercourse.
- Concentration Ranges: In adult men, testosterone levels range from 270 to 1070 ng/dL, averaging at 670 ng/dL, peaking in the 20s and decreasing slightly each year after age 40.
Understanding these hormonal functions is crucial for addressing issues related to fertility, such as erectile dysfunction and varicocele, which may be symptomatic of hormonal imbalances. Maintaining reproductive health and a healthy sperm count is closely tied to the balance of these hormones, highlighting the importance of hormonal equilibrium for overall male fertility.
Read: Causes of Low Sperm Count: Understanding the Factors
Key Hormones Involved in Male Fertility

Testosterone is a key male hormone that directly influences male fertility, primarily by regulating sperm production. Low testosterone levels, or hypogonadism, can still support sperm production but may be compromised due to factors such as age, obesity, injury to the testicles, and lifestyle choices including excessive alcohol and marijuana use. Chronic conditions like diabetes and treatments like chemotherapy also pose risks.
The hormonal hierarchy within the male reproductive system starts with Gonadotropin-releasing hormone (GnRH), which is the primary inducer of other critical hormones. It is produced in the hypothalamus and signals the pituitary gland to release Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH), both of which have direct roles in fertility:
FSH: Stimulates the testicles to produce sperm, crucial for maintaining adequate sperm count.
LH: Triggers testosterone production in the testicles, essential for sperm production and maintaining secondary male characteristics and sexual function.
Any disruption in the balance and interaction among these hormones—GnRH, FSH, LH, and testosterone—can lead to a range of reproductive issues, from subfertility to complete infertility. The complex interplay between these hormones is further influenced by the thyroidal and adrenal axes, which can modulate the Hypothalamic-pituitary-gonadal (HPG) axis, illustrating the intricate network and its susceptibility to hormonal imbalance.
Symptoms of Hormonal Imbalances in Men
Men experiencing hormonal imbalances often face a range of symptoms that can affect their daily lives and overall health. The primary male hormone, testosterone, plays a pivotal role in fertility and its deficiency can lead to several issues:
Sexual Health and Fertility:
- Decreased sperm production and low sperm count.
- Erectile dysfunction, making it challenging to engage in sexual activity.
- Reduced sex drive, resulting in less frequent intercourse.
Physical Well-being:
- Loss of muscle mass and decreased bone strength.
- Increased body fat, particularly around the abdomen.
- Symptoms such as facial puffiness, joint stiffness, and muscle aches.
Mental and Emotional Health:
- Cognitive decline and difficulty concentrating.
- Changes in mood, including depression and anxiety.
- Sleep disturbances, including insomnia.
Other notable symptoms include the development of breast tissue (gynecomastia), weakened bones potentially leading to osteoporosis, and a general decline in energy levels. These symptoms underscore the importance of hormones in regulating not only reproductive health but also metabolism, blood sugar, and stress levels. It’s crucial for men to be aware of these signs, as they can indicate underlying hormonal imbalances that may require medical attention to restore balance and maintain overall health.
Factors Impacting Male Hormones and Male Fertility
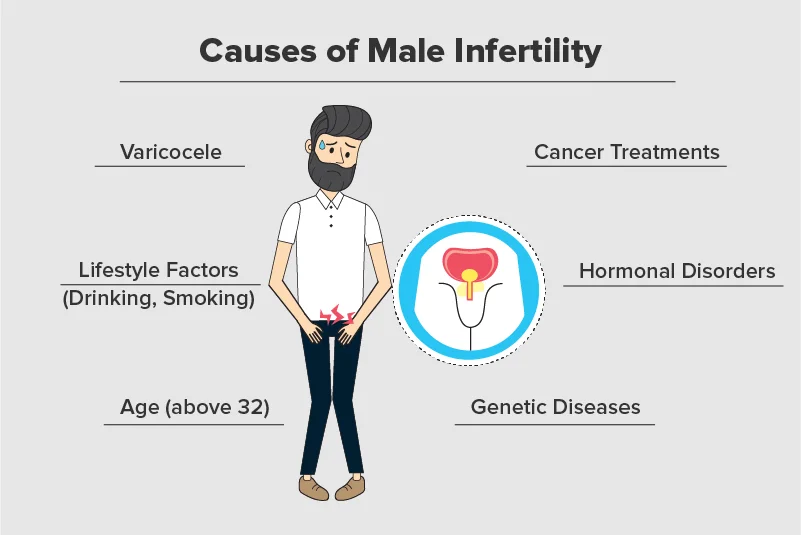
Testosterone, the key male hormone, is crucial for fertility, particularly in its role in sperm production. However, various factors can impact hormonal balance and, consequently, male fertility:
Health and Lifestyle Factors:
- Advancing age can naturally lower hormone levels.
- Obesity may lead to increased estrogen and lower testosterone levels.
- Testicular injuries can impair hormone production.
- Substance abuse, including excessive alcohol and chronic narcotic use, disrupts hormonal balance.
- Medical treatments like chemotherapy can have lasting effects on fertility.
Medical Conditions:
- Diabetes can affect testosterone levels and erectile function.
- Thyroid disorders, both hypothyroidism and hyperthyroidism, alter sex hormone-binding globulin (SHBG) and testosterone levels, affecting sperm maturation and quality.
- Pituitary gland issues can lead to hormonal imbalances, influencing LH and FSH production.
Environmental Influences:
- Exposure to Endocrine Disrupting Chemicals (EDCs) such as pesticides can affect the hypothalamic-pituitary-gonadal axis and disrupt hormone production.
- EDCs like phthalates and Bisphenol A (BPA) have been linked to reduced sperm quality and hormonal imbalances.
Maintaining reproductive health involves managing these factors through a healthy lifestyle, including a balanced diet, regular exercise, stress management, and avoiding harmful substances. It’s crucial to understand how these elements can affect hormonal balance and fertility to take proactive steps towards maintaining or improving reproductive health.
Strategies for Maintaining Hormonal Balance
To foster hormonal balance and enhance male fertility, consider the following strategies:
Lifestyle Adjustments:
- Quit smoking to potentially elevate testosterone levels.
- Achieve and maintain a moderate weight, as excess body fat can convert testosterone into estrogen.
- Incorporate regular strength training to boost libido and support normal testosterone levels.
Read: 10 Zinc Rich Foods That Boosts Your Immunity
Dietary Choices:
- Opt for a whole-food diet rich in Zinc, B Vitamins, and Essential Fatty Acids to support fertility and hormone function.
- Reduce sugar intake to maintain hormone function and prevent obesity and related diseases.
- Include healthy fats like MCTs and omega-3s to decrease insulin resistance and control appetite.
Environmental and Health Management:
- Minimize exposure to toxins by choosing filtered water, cleaner air, and hormone-friendly personal care products.
- Manage stress effectively as chronic stress elevates cortisol, potentially leading to insulin resistance and obesity.
- Ensure adequate, high-quality sleep, which is vital for hormonal equilibrium, including insulin, cortisol, leptin, ghrelin, and HGH.
Additionally, it’s crucial to be cautious with testosterone replacement therapy, as it may reduce sperm count and is not recommended for men wishing to conceive. Instead, medications like human chorionic gonadotropin (HCG) and clomiphene citrate can be considered under the guidance of a urologist with infertility expertise. True testosterone deficiency should be evaluated by a medical endocrinologist to safely increase levels without the use of testosterone supplements.
The Importance of Medical Consultation
Hormonal testing is a critical step for men facing infertility, as it assesses the levels of key hormones in the blood, pinpointing imbalances that could hinder successful reproduction. Consulting with a urologist who specializes in male reproductive and sexual health is vital for individuals trying to conceive, as they can offer comprehensive evaluations and guide appropriate treatment options. Bioidentical Hormone Replacement Therapy (BHRT) has emerged as a safe and effective means to restore hormonal balance in men, addressing issues that affect fertility.
When it comes to diagnosing and treating hormonal imbalances, medical consultation is indispensable. Treatment plans are tailored to the individual, depending on the root cause, and could range from hormone replacement therapy to medication, and in some cases, surgery or radiation therapy. Seeking professional healthcare advice ensures that hormonal imbalances are accurately diagnosed and effectively treated.
For those with a true testosterone deficiency, it’s essential to undergo a thorough evaluation by a medical endocrinologist. This ensures that testosterone levels are safely increased without resorting to supplements that could potentially reduce sperm count. Professional guidance helps in making informed decisions about treatment options that best support reproductive health and sperm count.
Conclusion
In synthesizing the discussions held within this article, we affirm the vital role hormones play in male fertility. The delicate balance of testosterone, FSH, LH, and other hormones is foundational for reproductive health, and disturbances can significantly disrupt fertility. Our exploration has illuminated the intertwining factors that affect hormonal equilibrium, from lifestyle choices and medical conditions to environmental influences, all contributing to the complex tapestry of male reproductive health.
Taking proactive steps to maintain this balance ensures a greater likelihood of preserving fertility, with lifestyle adjustments, diet, and stress management as cornerstones of such efforts. Through informed strategies and expert guidance, men can work towards achieving a harmonious hormonal state, underpinning both their reproductive capabilities and overarching well-being.


