Ever wonder why after a 15-mile walking day, everything hurts? Not just the expected sore calves, but mysterious knee pain, unexpected hip discomfort, and foot aches that weren’t there yesterday.
Walking seems so natural and harmless—until it’s not. Those daily steps add up, and without proper preparation, they can lead to significant walking injuries that sideline even the most dedicated fitness enthusiasts.
The human body wasn’t designed for the concrete jungles and marathon shopping trips of modern life. Walking injuries from overuse don’t just happen to athletes or hikers tackling challenging terrain.
But here’s the question nobody’s asking: what’s happening in your body with each of those 10,000 daily steps? The answer might surprise even seasoned walkers.
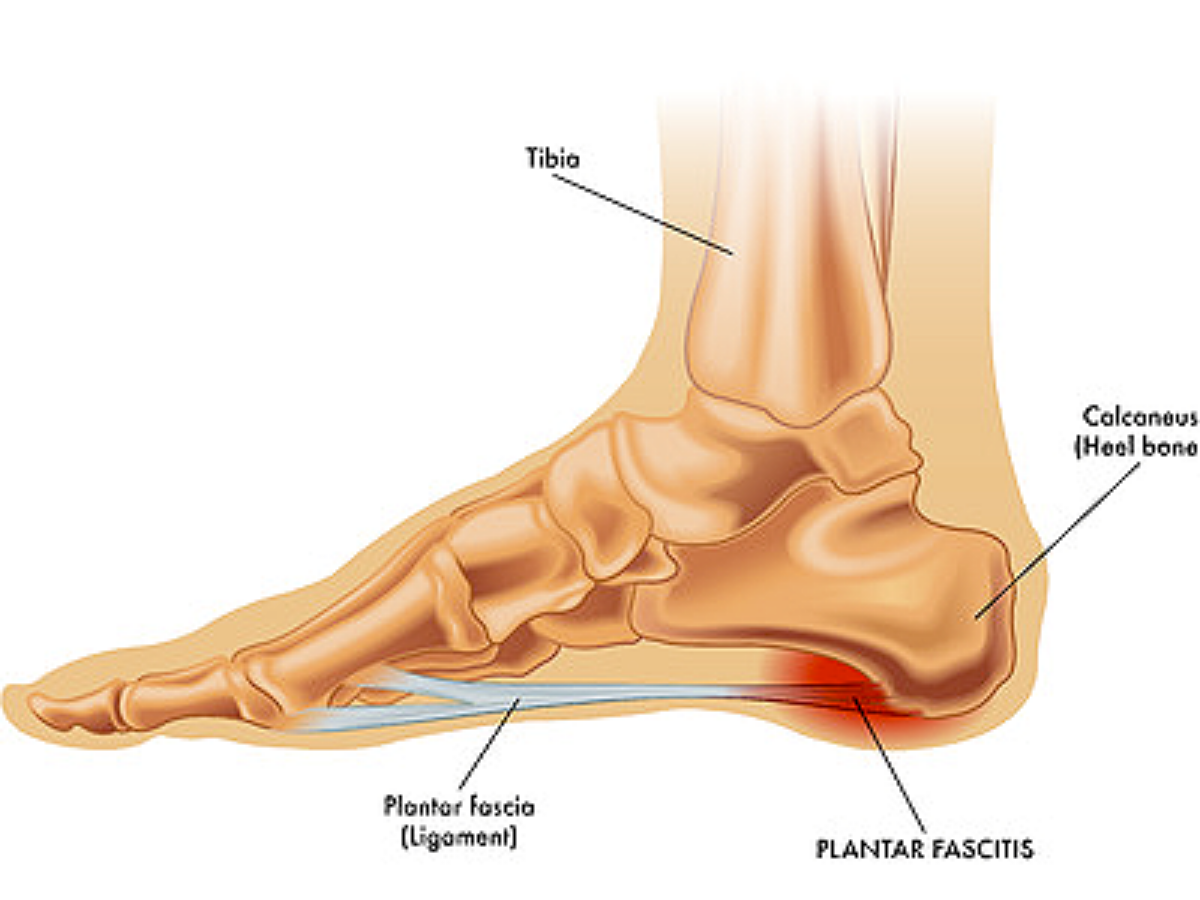
A. Plantar Fasciitis: Understanding the Painful Heel Condition
Plantar fasciitis ranks among the most common foot injuries walkers experience when pushing too far. This painful condition develops when the plantar fascia—the thick band of tissue connecting your heel to your toes—becomes inflamed. The telltale sign? A sharp, stabbing pain with the first steps in the morning that might ease during the day but returns after standing or walking for extended periods.
Excessive walking puts repetitive stress on this tissue, especially when:
Walking on hard surfaces
Wearing shoes with poor arch support
Increasing mileage too quickly
Walking mechanics also play a crucial role, as overpronation (rolling the foot inward too much) can overstretch the fascia. Rest helps, but doesn’t address the root cause. Most walkers find relief through:
Regular stretching of calf muscles and the plantar fascia
Ice massage after walking
Wearing supportive shoes with proper arch support
Using night splints to keep the fascia stretched overnight
Gradual return to walking with modified distance
B. Stress Fractures: Small Cracks with Big Consequences
Stress fractures develop as tiny cracks in bones from repetitive force—not from a single traumatic event. For walkers, these hairline fractures typically affect the metatarsals (the long bones in the foot) or the lower leg bones.
The danger lies in how these injuries develop gradually. Many walkers ignore the initial mild pain, continuing their routine until the discomfort becomes unbearable. By then, recovery time has already doubled or tripled.
Risk factors include:
Sudden increases in walking distance or intensity
Walking on uneven or hard surfaces
Poor footwear with inadequate shock absorption
Low bone density or nutritional deficiencies
Unlike muscle soreness that improves during activity, stress fracture pain typically worsens throughout a walk and feels better with rest. The affected area might show swelling or tenderness when pressed.
Recovery requires:
Complete rest from weight-bearing activity (4-8 weeks)
Possible use of a walking boot or crutches
Gradual return using the 10% rule: increase distance by no more than 10% weekly
C. Blisters and Calluses: Prevention and Treatment
While seemingly minor compared to other foot injuries, blisters can derail a walking routine just as effectively. These fluid-filled sacs form when friction creates a separation between layers of skin. Hot spots—areas of redness before blister formation—serve as early warning signals.
Prevention strategies work better than treatment:
Properly fitted shoes with minimal movement inside
Moisture-wicking socks (avoid cotton)
Lubricants or anti-friction products on problem areas
Gradual breaking-in of new footwear
Calluses represent the body’s defensive response to repeated pressure or friction. While providing natural protection, excessively thick calluses can become painful and crack. Regular maintenance with pumice stones or foot files prevents buildup.
For existing blisters:
Small blisters: Leave intact if possible, cover with moleskin or blister bandages
Large, painful blisters: Clean with antiseptic, drain with sterilized needle, apply antibiotic ointment
Never remove the “roof” of a blister—it provides natural protection against infection
D. Morton’s Neuroma: When Nerves Get Compressed
Morton’s neuroma develops when tissue thickens around a nerve between the metatarsal bones, typically between the third and fourth toes. This benign growth causes burning pain, tingling, and numbness that often worsens during walking.
Excessive walking contributes to this condition when combined with:
Narrow or tight footwear that squeezes toes together
High-heeled shoes that increase pressure on the forefoot
Foot deformities like bunions or hammertoes
Certain high-impact activities
The sensation often feels like standing on a pebble or having a fold in the sock. Many walkers describe a burning pain that radiates into the toes, sometimes with a clicking sensation.
Conservative treatment approaches include:
Switching to wider, lower-heeled shoes with ample toe box space
Using metatarsal pads to spread the bones and reduce pressure
Taking breaks to massage the affected area during long walks
Anti-inflammatory medications to reduce pain and swelling
More severe cases might require corticosteroid injections or, rarely, surgical removal of the affected nerve.
E. Bunions and Hammertoes: Structural Problems That Worsen with Overuse
Bunions (hallux valgus) appear as bony bumps at the base of the big toe, causing the toe to angle toward the smaller toes. While genetics plays a significant role in their development, excessive walking in improper footwear accelerates progression and pain.
Hammertoes develop when the middle joint of a toe bends abnormally, creating a hammer-like appearance. Both conditions share common risk factors:
Tight, narrow shoes that crowd toes
Flat feet or abnormal foot mechanics
Underlying arthritis
Hereditary factors
The pain from these conditions intensifies with each step during long walks, as friction against shoes creates inflammation and potentially painful corns.
Management strategies include:
Shoes with wide toe boxes and proper arch support
Toe spacers or padding to reduce pressure and friction
Toe exercises to maintain flexibility and strength
Ice after walking to reduce inflammation
Splints to help realign toes (particularly for early hammertoes)
For severe cases unresponsive to conservative approaches, surgical correction might be necessary to realign the affected joints and relieve persistent pain.
Lower Body Impact Injuries
A. Shin Splints: Causes and Recovery Strategies
Shin splints strike when you’ve pushed those walks too far. This painful condition (medically known as medial tibial stress syndrome) shows up as pain along the inner edge of the shinbone. The primary culprit? Repetitive stress on the shinbone and surrounding tissues.
Walking on hard surfaces, wearing worn-out shoes, or suddenly increasing walking distance can trigger shin splints. The pain typically starts as a dull ache that intensifies during activity.
Recovery requires a multi-faceted approach:
Rest is non-negotiable – take a break from walking or significantly reduce mileage
Ice the affected area for 15-20 minutes several times daily
Compression sleeves can provide relief during recovery
Proper footwear with adequate arch support is crucial
Prevention strategies include gradually increasing walking distance (no more than 10% weekly), strengthening calf muscles, and incorporating proper warm-up routines before walks.
B. Knee Pain and Patellofemoral Syndrome
Knee pain ranks among the most common complaints from avid walkers. Patellofemoral syndrome—often called “walker’s knee”—occurs when the kneecap doesn’t track properly over the femur during movement.
The telltale sign? Pain around or behind the kneecap that worsens when walking uphill, climbing stairs, or sitting with bent knees for extended periods.
This condition stems from several factors:
Muscle imbalances (particularly weak quadriceps)
Improper walking mechanics
Flat feet or high arches
Inadequate footwear
Treatment typically involves:
Temporarily modifying walking routine
Strengthening exercises focusing on quadriceps
Stretching tight muscles that pull on the knee
Using supportive insoles or orthotics
C. Hip Bursitis: When Your Joints Protest
Hip bursitis develops when the fluid-filled sacs (bursae) cushioning the hip joint become inflamed. Excessive walking creates friction between tissues in this area, leading to pain that radiates from the hip to the outside of the thigh.
The pain typically intensifies when:
Lying on the affected side
Walking up inclines
After prolonged sitting followed by activity
Treatment approaches include:
Anti-inflammatory medications to reduce swelling
Physical therapy focusing on hip strengthening
Temporary activity modification
Ice therapy after walking
In severe cases, corticosteroid injections
Long-term prevention requires proper hip-strengthening exercises, particularly targeting the gluteal muscles that stabilize the hip during walking.
D. IT Band Syndrome: The Side-of-Knee Nemesis
The iliotibial (IT) band runs from the hip to just below the knee along the outside of the thigh. When this thick band becomes inflamed from overuse, IT band syndrome develops.
Symptoms include sharp pain on the outside of the knee that often starts after a specific time or distance of walking. The pain may disappear during rest but returns quickly once walking resumes.
Common causes include:
Walking on uneven surfaces or consistently on one side of a crowned road
Poor walking mechanics
Leg length discrepancies
Inadequate warm-up or cool-down
Effective recovery strategies include:
Foam rolling the IT band (though painful, it’s effective)
Stretching the IT band and surrounding muscles
Strengthening hip abductors and core muscles
Ensuring proper footwear with adequate support
Temporarily reducing walking distance and intensity
Warning Signs You’re Walking Too Much
A. Persistent Pain That Worsens During Activity
Walking is generally healthy, but when the body screams, it’s time to listen. Persistent pain that intensifies during walking isn’t just an inconvenience—it’s a warning flag from the body.
The key difference between normal exercise discomfort and problematic pain? Normal muscle soreness typically subsides as the body warms up. In contrast, pain that gets worse as activity continues signals potential damage occurring.
Common problem areas include:
Foot arch (plantar fasciitis)
Shin splints
Knee joints
Hip flexors
Lower back
Pain that persists for more than 72 hours after walking deserves attention. The body needs recovery time, and continuing to push through pain can transform a minor issue into a serious injury requiring months of rehabilitation.
B. Declining Performance Despite Consistent Training
Noticed walking feels harder despite maintaining the same routine? This paradoxical decline in performance often indicates overtraining. The body simply hasn’t had adequate recovery time between walking sessions.
Signs of overtraining include:
Taking longer to complete usual routes
Feeling unusually fatigued during walks
Needing more recovery time between sessions
Decreased motivation to walk
Elevated resting heart rate
This performance decline happens when muscles, tendons, and joints accumulate micro-damage faster than the body can repair them. The solution isn’t always to push harder—sometimes backing off intensity or adding rest days proves more effective for long-term progress.
C. Unusual Swelling or Joint Stiffness
Swelling around joints after walking isn’t normal, particularly when it persists hours after activity ends. This inflammation response indicates tissues are under excessive stress.
Pay particular attention to:
Ankle swelling that leaves indentations when pressed
Knee joints feeling tight or locked
Toes that appear puffy or discolored
Joint stiffness that’s worse in the morning
Reduced range of motion in affected areas
Morning stiffness lasting longer than 30 minutes warrants special attention. While some initial stiffness upon waking is normal, prolonged morning discomfort suggests inflammation hasn’t resolved overnight.
D. Changes in Gait or Walking Mechanics
The body compensates for pain in fascinating but potentially harmful ways. Subtle changes in walking pattern often develop unconsciously to avoid pain in overused areas.
Watch for these telling signs:
Limping or favoring one side
Shortened stride length
Decreased arm swing
Foot turning outward or inward more than usual
Excessive pronation (foot rolling inward)
These compensatory patterns create a dangerous cycle—the altered mechanics place abnormal stress on different body parts, potentially causing secondary injuries. Walking in front of a mirror or recording a short video can help identify these subtle changes before they cause additional problems.
Wrapping Up Your Walking Journey
Walking represents a cornerstone of physical fitness, but like any exercise, moderation remains key. Excessive walking can lead to various foot injuries including plantar fasciitis, blisters, and stress fractures, while the lower body may suffer from shin splints, knee pain, and hip discomfort. Recognizing warning signs such as persistent pain, decreased performance, fatigue, and mood changes allows individuals to adjust their walking routine before serious damage occurs.
Maintaining a balanced approach to walking involves proper footwear, gradual intensity increases, and incorporating rest days. Those experiencing symptoms of overuse should consult healthcare professionals rather than pushing through pain. By respecting physical limitations and practicing proper walking techniques, walking can remain a sustainable, beneficial activity without the negative consequences of overexertion.