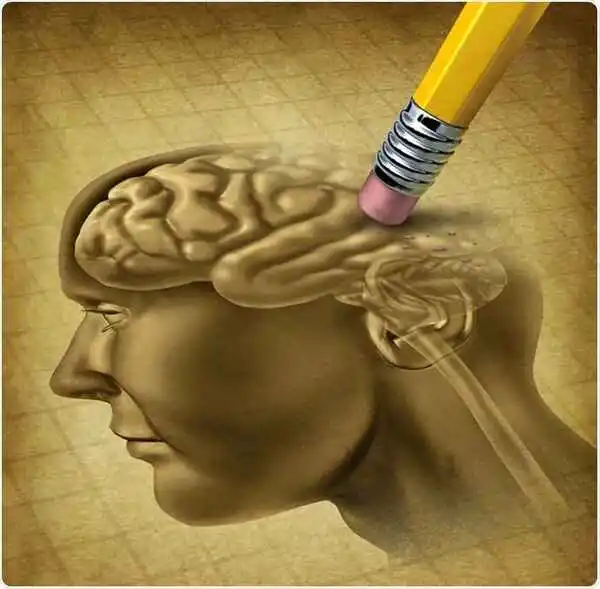
Alzheimer’s disease leads to a progressive decline in memory, thinking, learning, and organizational skills. It is the most common cause of dementia, typically affecting individuals over the age of 65. While there is no cure, certain medications and therapies can help manage symptoms temporarily.
Named after Dr. Alois Alzheimer, who first described it in 1906, Alzheimer’s disease initially presents with mild symptoms that worsen over time. Common symptoms include memory loss, language difficulties, and impulsive or unpredictable behavior.
Key features of Alzheimer’s include the presence of plaques and tangles in the brain, and a loss of connections between neurons. These changes hinder the transmission of information within the brain and between the brain and the body.
As the disease progresses, individuals find it increasingly difficult to remember recent events, reason, and recognize familiar people.
Signs and Symptoms of Alzheimer’s Disease
The symptoms of Alzheimer’s disease (AD) vary depending on the stage of the condition. Generally, AD involves a gradual decline in:
- Memory
- Reasoning and handling complex tasks
- Language
- Understanding visual and spatial relationships
- Behavior and personality
People with Alzheimer’s may not recognize their mental decline, but these signs are often noticeable to loved ones. Anyone experiencing dementia-like symptoms should consult a healthcare provider promptly.
Read This: 10 Essential Tips on How to Keep Your Brain Healthy After 50
Mild Stage Symptoms
In the mild stage, symptoms become noticeable. The most common early symptom is forgetting newly learned information, such as recent events, places, and names. Other symptoms include:
- Difficulty finding the right words
- Frequently losing or misplacing objects
- Trouble making plans or organizing
- Difficulty problem-solving
- Taking longer to complete routine tasks
Most individuals in this stage can still recognize familiar faces and navigate familiar places.
Moderate Stage Symptoms
The moderate stage is typically the longest and can last for many years. People in this stage often require care and assistance. Symptoms include:
- Increased memory loss and confusion
- Growing disorientation about time and place
- Poor short-term memory
- Difficulty recognizing friends and family
- Repeating stories or thoughts
- Difficulty with simple math
- Needing help with self-care tasks
- Personality changes, such as agitation, depression, apathy, or anxiety
- Groundless suspicions about loved ones (delusions)
- Urinary and/or fecal incontinence
- Sleep disturbances
- Wandering from their living area
Severe Stage Symptoms
In the final stage of Alzheimer’s, dementia symptoms become extremely severe, requiring extensive care. Individuals in this stage often:
- Experience almost total memory loss.
- Are unaware of their surroundings.
- Need assistance with all basic daily activities, such as eating, sitting up, and walking.
- Lose the ability to communicate, with speech limited to a few words or phrases.
- Become highly vulnerable to infections, particularly pneumonia and skin infections.
At this stage, hospice care may be appropriate to ensure comfort.

Causes
Alzheimer’s disease, like all types of dementia, results from the death of brain cells. It is a neurodegenerative condition, meaning brain cell death occurs progressively over time. In Alzheimer’s, brain tissue gradually loses nerve cells and connections, while tiny deposits known as plaques and tangles accumulate on the nerve tissue.
- Plaques form between dying brain cells and are composed of a protein called beta-amyloid.
- Tangles occur within nerve cells and are made from a protein called tau.
The exact reasons for these changes are not fully understood, but several factors may contribute. The Alzheimer’s Association provides a visual guide to illustrate the development of Alzheimer’s disease.
Stages of Alzheimer’s Disease
Healthcare providers and organizations use various terms to describe the stages of Alzheimer’s disease based on symptoms. Although the terminology may differ, the stages follow a similar pattern of progressively worsening symptoms. Each person with Alzheimer’s progresses through the stages at different rates, and not all changes occur in every individual. Stages may also overlap, making it challenging to place someone in a specific stage.
Some common frameworks for describing the stages include:
- Preclinical Alzheimer’s Disease
- Mild Cognitive Impairment (MCI) due to Alzheimer’s Disease
- Mild Dementia due to Alzheimer’s Disease
- Moderate Dementia due to Alzheimer’s Disease
- Severe Dementia due to Alzheimer’s Disease
Alternatively, stages can be broadly categorized as:
- Mild
- Moderate
- Severe
Or:
- Early
- Middle
- Late
Preclinical Alzheimer’s Disease
The preclinical stage is typically referenced in research and involves no noticeable symptoms (asymptomatic). However, changes are occurring in the brain, which can last for years or even decades. People in this stage are not usually diagnosed with Alzheimer’s because they function at a high level. Brain imaging tests can now detect amyloid deposits that interfere with brain communication before symptoms begin.
Mild Cognitive Impairment (MCI) due to Alzheimer’s Disease
When memory problems become noticeable, healthcare providers may identify it as mild cognitive impairment (MCI), a slight decline in mental abilities compared to others of the same age. Early-stage Alzheimer’s may present as minor declines in abilities, noticeable to the individual or close associates, but not severe enough to interfere with daily life. In some cases, treatable illnesses can cause MCI, but for most, it is a step towards dementia. Researchers view MCI as the stage between normal aging and early-stage dementia. Multiple conditions can lead to MCI, such as Alzheimer’s or Parkinson’s disease. Likewise, dementia can arise from several different factors.

Dementia is an umbrella term for a range of conditions characterized by a decline in cognitive functioning. It encompasses various types of cognitive impairments that affect memory, thinking, and social abilities severely enough to interfere with daily life.
Alzheimer’s disease is the most common type of dementia. It is marked by the formation of plaques and tangles in the brain, leading to a gradual decline in cognitive function and language abilities. Symptoms typically start slowly and worsen over time.
Other types of dementia include:
- Huntington’s disease
- Parkinson’s disease
- Creutzfeldt-Jakob disease
It is possible for a person to have more than one type of dementia.
Diagnosis
To diagnose Alzheimer’s disease, a person must exhibit memory loss, cognitive decline, or behavioral changes that impact their daily functioning. Often, friends and family notice these symptoms before the individual does.
There is no single test for Alzheimer’s. Diagnosis typically involves:
- Cognitive and memory tests to assess thinking and memory abilities
- Neurological function tests to evaluate balance, senses, and reflexes
- Blood or urine tests
- CT or MRI scans of the brain
- Genetic testing
Assessment tools are available to evaluate cognitive function, and in some cases, genetic testing may be appropriate, especially if the dementia is related to an inherited condition like Huntington’s disease. Certain forms of the APOE e4 gene are linked to a higher risk of developing Alzheimer’s.
What’s the Treatment?
While there is no cure for Alzheimer’s disease, certain medications can temporarily slow the progression of dementia symptoms and help manage behavioral symptoms. Early treatment can help maintain daily functioning for a while, but current medications cannot stop or reverse the disease.
Treatment is highly individualized, and healthcare providers work closely with patients and their caregivers to develop the best plan. The U.S. Food and Drug Administration (FDA) has approved two types of drugs for treating Alzheimer’s symptoms:
- Cholinesterase inhibitors: Donepezil (Aricept®), Rivastigmine (Exelon®), and Galantamine (Razadyne®) help treat mild to moderate Alzheimer’s by blocking the enzyme that breaks down acetylcholine, a chemical that aids nerve cell communication.
- NMDA antagonists: Memantine (Namenda®) is used for moderate to severe Alzheimer’s and helps keep certain brain cells healthier. Research indicates that individuals with Alzheimer’s who use memantine exhibit improved performance in essential daily tasks, including eating, walking, using the toilet, bathing, and dressing.
The FDA has also given accelerated approval for aducanumab (Aduhelm™), the first disease-modifying therapy for Alzheimer’s, which helps reduce amyloid deposits in the brain. However, it may only be effective for those in the early stages of the disease.

What are the 7 stages of Alzheimer’s?
The following are the 7 clinical stages of Alzheimer’s disease:
Stage 1: A person appears cognitively normal, but pathological changes are happening in the brain.
Stage 2: Prodromal stage: mild memory loss, but generally this is indistinguishable from normal forgetfulness.
Stage 3: Progression into mild cognitive impairment (MCI). Individuals may get lost or have difficulty in finding correct wording.
Stage 4: Moderate dementia; poor short-term memory. Individuals forget some of their personal history.
Stage 5: Cognition continues to decline, and at this point, individuals need help in their daily lives. They suffer from confusion and forget many personal details.
Stage 6: Severe dementia. Requiring constant supervision and care. Patients fail to recognize many of their family and friends and have personality changes.
Stage 7: Individuals are nearing death. They show motor symptoms, have difficulty communicating, are incontinent, and require assistance in feeding.
What is the life expectancy for Alzheimer’s?
According to the Alzheimer’s Association, on average, a person with the condition will live four to eight years after diagnosis. Depending on other factors, though, they may live as long as 20 years.
Alzheimer’s disease is a neurodegenerative condition. A buildup of plaques and tangles in the brain, along with cell death, causes memory loss and cognitive decline.
There is currently no cure, but drugs and other treatments can help slow or ease the cognitive, emotional, and behavioral symptoms and improve the person’s quality of life.