High protein diet have surged in popularity for their role in weight loss and improving cardiometabolic parameters, yet their effects on cardiovascular health remain a contentious topic. Despite a meta-analysis indicating no significant difference in cardiovascular risks compared to normal protein diets, it is essential to scrutinize the underlying implications of sustained high protein intake on heart health. As research delves deeper into what happens if you eat too much protein, individuals must consider the balance between the immediate benefits of high-protein foods and potential too much protein symptoms that emerge over time.
This article aims to dissect the complex relationship between high protein diets and cardiovascular risks, with a focus on protein sources and their impacts on heart disease. In our discussion, we will navigate through the nuances of atherosclerosis, the role of specific amino acids like leucine in arterial health, and compare plant versus animal proteins. By investigating how much protein individuals need and examining the safer ways to consume protein, readers will gain a comprehensive understanding of making high-protein diets heart-healthy, the necessary monitoring of saturated fat intake, and the importance of whole foods in mitigating the risks.
Understanding Atherosclerosis and Protein Intake
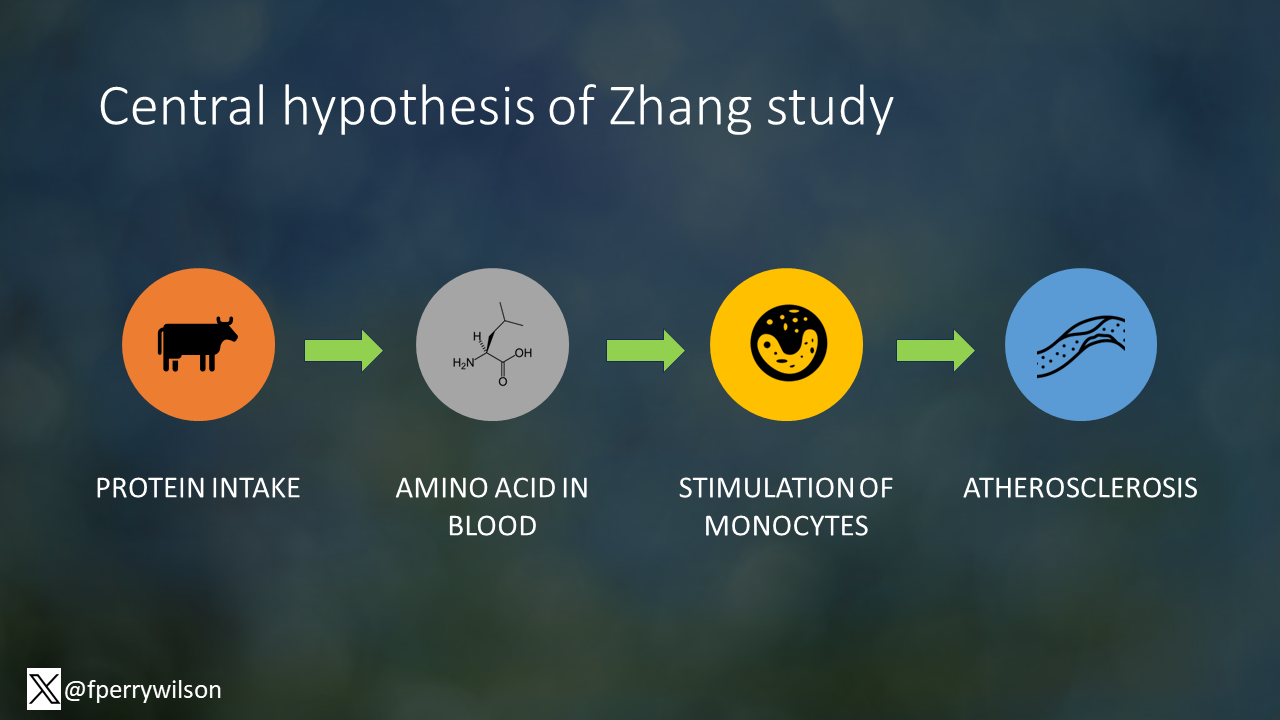
High-protein diets, often lauded for their weight loss benefits, may inadvertently elevate cardiovascular risk. This elevation is linked to the activation of macrophage mammalian target of rapamycin (mTOR), a cellular pathway that, when overstimulated, can suppress the natural cellular cleaning process known as mitophagy. This suppression may contribute to the progression of atherosclerosis, a condition characterized by the accumulation of plaques within arterial walls.
- Macrophage mTOR Activation: Research indicates that diets consisting of over 22% of calories from protein can heighten the activity of immune cells that are instrumental in forming atherosclerotic plaques. The macrophages, when triggered by excessive protein, can drive the risk of cardiovascular diseases.
- Inflammatory Response: High protein intake, particularly from animal sources rich in certain amino acids like leucine, can instigate an inflammatory response in white blood cells. This inflammation, along with other risk factors such as high cholesterol and high blood pressure, may contribute to heart attack risk.
- Atherosclerosis and Protein Sources: Studies have shown that high protein diets, especially when combined with high fat intake, can promote the development of atherosclerosis. Mice on a high-fat, high-protein diet developed about 30% more arterial plaque than those on a high-fat, low-protein diet. The plaques in the high-protein group were also more likely to be unstable, which increases the risk of blockages and subsequent heart attacks.
By understanding these mechanisms, individuals can better gauge how much protein they need and make informed decisions about protein sources, considering the balance between high-protein foods, whole foods, and saturated fat intake to mitigate heart disease risk.
The Role of Leucine in Arterial Damage
Leucine, an amino acid prevalent in animal-based proteins, plays a crucial role in cardiovascular health. It is involved in various metabolic pathways that can either promote or inhibit atherosclerosis, a leading cause of heart disease. Here is how leucine influences arterial health:
Pathological Pathways:
- Leucine has been linked to the activation of pathways that can lead to atherosclerosis. Its abundance in animal-derived foods suggests a potential risk factor for those consuming high levels of these proteins.
- The amino acid is known to affect macrophage function, cells that contribute to plaque formation in arteries, potentially heightening cardiovascular disease risk.
Protective Mechanisms:
- Contrarily, leucine has shown protective effects against atherosclerosis. A study identified it as one of six amino acids that significantly reduced lipid accumulation in arterial cells, thus protecting against the disease.
- Moreover, leucine modifies macrophage lipid metabolism and enhances mitochondrial respiration, which inhibits foam cell formation and atherogenesis.
Supplementation Outcomes:
- Leucine supplementation in apoE null mice resulted in a notable reduction of atherosclerotic lesions and improvements in lipid profiles, with decreased LDL-C and increased HDL-C levels.
- It also regulates gene expression related to cholesterol efflux and reduces systemic inflammation, showcasing its potential in attenuating atherosclerosis.
Incorporating too much protein, particularly from animal sources, into one’s diet without considering the source and quantity can lead to adverse cardiovascular effects. However, understanding the role of leucine and its impact on heart health can guide adjustments in protein intake to support cardiovascular function.
Read : The Boiled Egg Diet: Is It a Weight Loss Wonder or a Health Hazard?
Plant vs. Animal Protein: Effects on Cardiovascular Health

In the context of cardiovascular health, the distinction between animal and plant proteins is significant. A varied diet that includes plant-based proteins can offer cardiovascular benefits:
- Diverse Protein Sources: Embracing a range of protein sources, especially plant-based options like legumes, nuts, and seeds, can have a favorable impact on heart health. This diversity not only provides a broad spectrum of essential nutrients but also introduces dietary fibers and phytochemicals that are absent in animal proteins.
- Plant Proteins and Heart Disease Risk: Consuming plant proteins such as beans, whole grains, and vegetables is linked to a healthier heart. A systematic review of studies suggests that replacing animal protein with plant protein is associated with lower cardiovascular disease (CVD) mortality and a reduced incidence of Type 2 Diabetes (T2D). The protective effect of plant protein is considered ‘limited-suggestive’ for both CVD mortality and T2D incidence.
- Health Benefits of Plant-Based Diets: Diets rich in nutrient-dense plant foods are correlated with a decreased risk of developing T2D. Moreover, individuals adhering to a vegetarian diet typically have lower body weight, cholesterol levels, and a reduced risk of stroke, cancer, and death from heart disease compared to meat-eaters. Plant-based diets have also been connected to significant reductions in blood pressure when compared to diets high in animal protein.
Incorporating these findings into dietary choices, particularly by increasing the intake of plant-based proteins, aligns with a public health strategy to mitigate the risks of CVD and T2D. This approach not only addresses individual health concerns but also considers sustainability and the broader impact on public health.
Potential Benefits vs. Risks of High Protein Diets
High-protein diets are often sought for their potential to promote weight loss, increase muscle mass, and improve cardiometabolic parameters. Yet, their long-term impact on cardiovascular health is an area of active research, with studies revealing both benefits and risks.
Benefits of High-Protein Diets:
- Weight Management: High-protein foods may enhance satiety, which can lead to reduced calorie intake and aid in weight loss.
- Muscle Mass: Adequate protein intake is critical for the maintenance and growth of muscle mass, particularly in conjunction with exercise.
- Cardiometabolic Health: Some studies have shown improvements in biomarkers such as glycosylated hemoglobin, cholesterol levels, and blood pressure in patients with heart failure and diabetes following a high-protein diet.
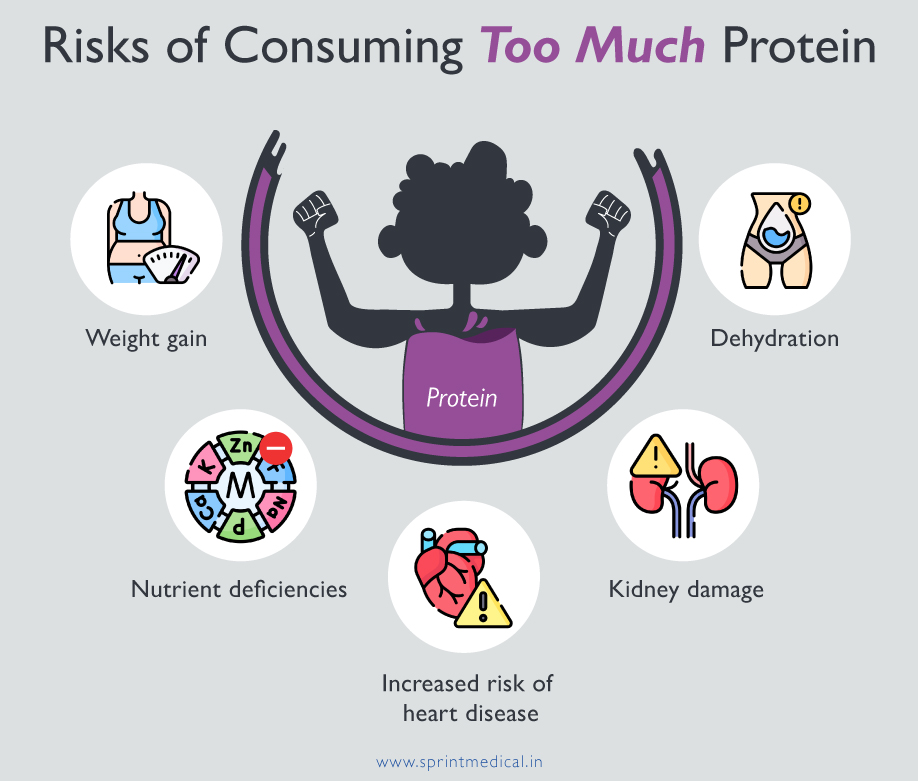
Risks Associated with High-Protein Diets:
- Atherosclerosis Progression: Excessive protein can stimulate macrophage mTOR signaling in atherosclerotic plaques, potentially leading to increased lesion complexity.
- Metabolic Concerns: High protein intake has been linked to unfavorable metabolic effects and a higher risk of type 2 diabetes mellitus (T2DM), cardiovascular, and renal outcomes.
- Nutrient Deficiency: Long-term adherence to high-protein diets without proper balance may result in deficiencies in other nutrients or fiber, leading to a range of health issues.
Mitigating Risks:
- Protein Source Selection: To reduce potential health risks, it is advisable to choose proteins wisely by incorporating whole foods, such as soy protein, beans, nuts, and lean cuts of meat, and avoiding processed meats.
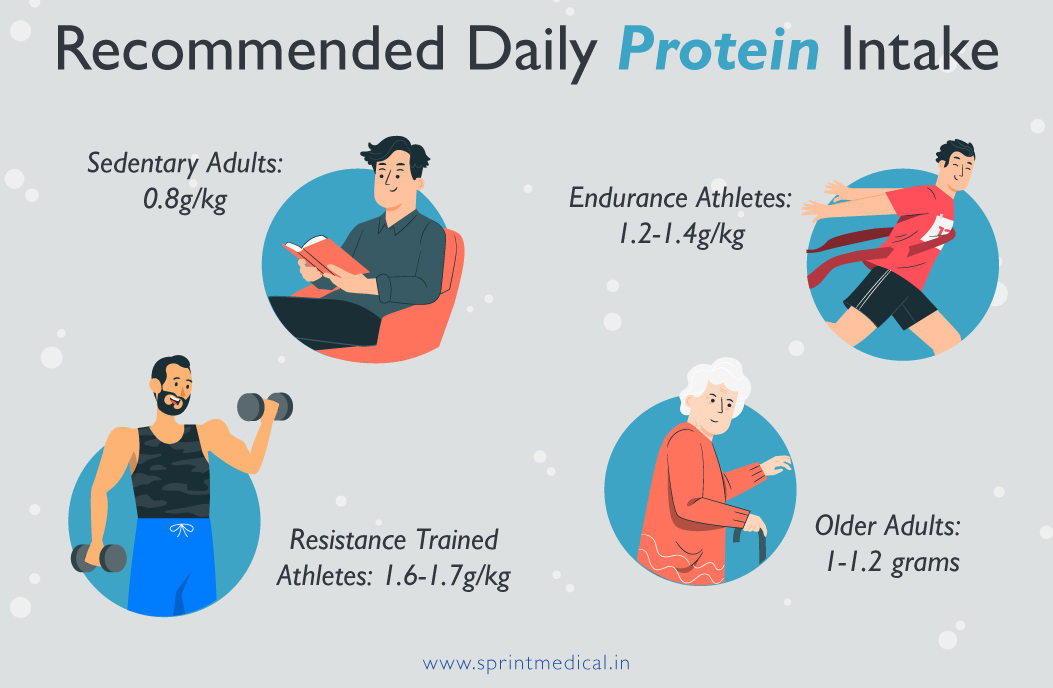
- Balanced Intake: Understanding how much protein one needs and adhering to guidelines, such as the RDA of 0.8 g/kg for the general adult population, can help maintain a healthy balance.
In conclusion, while high-protein diets may offer certain health benefits, it is crucial to approach them with caution, considering both the type and quantity of protein consumed. Further research is necessary to fully understand the implications of too much protein and to establish clear guidelines for protein intake that optimize health outcomes.
Adjusting Protein Intake for Heart Health
When considering adjustments to protein intake for heart health, it is crucial to take into account individual dietary needs, pre-existing health conditions, and the balance of other macronutrients. Here are some guidelines to help tailor protein consumption to support cardiovascular health:
Assessing and Adjusting Protein Intake
- Evaluate Current Consumption: Begin by assessing your current protein intake. Keep a food diary or use a nutrition tracking app to calculate daily protein consumption from all sources.
- Daily Protein Limits: The Dietary Reference Intake recommends limiting protein to 46 grams for women and 56 grams for men per day. Adjust your intake to stay within these limits.
- Protein Quality: Opt for high-quality protein sources such as fish, poultry, eggs, and dairy. These sources provide essential amino acids without the added saturated fats often found in processed meats.
Balancing Macronutrients
- Moderation is Key: Aim for a moderate protein intake, where 15-20% of your daily calories come from protein. This allows room for other essential macronutrients.
- Carbohydrates and Fats: Ensure your diet includes appropriate carbohydrate and fat intake. Focus on high-fiber, nutrient-rich carbohydrates like whole grains, vegetables, and fruits.
Practical Tips for Heart-Healthy Protein Choices
- Lean Protein Selection: Choose lean meats, skim milk, and other low-fat options that are high in protein.
- Combine Proteins with Vegetables: Create dishes that incorporate both meat and vegetables to balance your meal.
- Portion Control: Pay attention to portion sizes, aiming for 2- to 3-ounce servings of meat.
- Healthy Alternatives: For appetizers, opt for a plate of raw vegetables instead of high-fat cheese plates.
By regularly reassessing protein intake and making informed choices about protein sources, individuals can maintain a balanced diet that supports overall and cardiovascular health. Remember that the recommended daily allowance (RDA) for protein is a guideline, and the specific amount you need may vary based on factors such as age, weight, and activity level.
Conclusion
Through the lens of our in-depth exploration, it is clear that while high-protein diets can be beneficial for weight management and muscle growth, they must be approached with a nuanced understanding of their potential cardiovascular effects. A careful balance between the advantages and the cardiovascular risks associated with such diets is imperative, with emphasis on the quality and sources of protein consumed. The discerning selection of protein sources, particularly incorporating plant-based options, can be a heart-healthy strategy that caters to both individual wellness and broader public health concerns.
As we continue to navigate the complexities of dietary impacts on cardiovascular health, it becomes evident that moderation and informed choices are key. Adopting a diet that is attentively tailored to individual health needs, while aligning with nutritional guidelines, offers a robust foundation for maintaining cardiovascular well-being.
FAQs
Q: In what way can a high protein diet lead to heart disease?
A: Diets high in protein often include substantial amounts of saturated fat, which can cause blocked arteries (atherosclerosis) and an increase in LDL cholesterol, commonly known as “bad” cholesterol. These conditions are associated with an elevated risk of heart disease.Q: What are two potential health risks associated with a high protein diet?
A: Consuming high amounts of protein over a prolonged period can lead to health issues such as bone mineral loss and kidney damage. However, in individuals who are otherwise healthy, there is little evidence to suggest that a high protein intake is harmful.Q: What are some negative effects of consuming excessive protein?
A: Eating too much protein can result in a variety of problems, including weight gain (often short-term), bad breath, constipation, diarrhea, dehydration, kidney damage, an increased risk of cancer, and heart disease.Q: Is it possible for a high protein diet to affect your heart rate?
A: Yes, excessive protein consumption can lead to plaque build-up in the arteries and disturbances in heart rhythm. Some young people who use protein supplements and steroids without proper guidance have reported chest discomfort, rapid heart rates of around 120 beats per minute, dizziness, and palpitations.


