While morning sickness is a common hurdle for up to 80% of expecting individuals, Hyperemesis Gravidarum (HG) is a severe pregnancy complication characterized by extreme nausea and vomiting. Misidentified often as prolonged morning sickness, HG impacts less than 3% of pregnancies but poses a risk of dehydration, malnourishment, and significant weight loss.
This article delves into understanding hyperemesis gravidarum, its causes, and risk factors, the potential impact on health and pregnancy, and the options available for managing and treating this debilitating condition. Acknowledging the differences between common pregnancy symptoms and HG is crucial for the well-being of both the mother and the fetus.
Understanding Hyperemesis Gravidarum

Hyperemesis gravidarum (HG) is a condition that occurs during pregnancy, characterized by severe nausea and vomiting. Unlike typical morning sickness, which usually abates after the first trimester, HG can persist throughout the entire pregnancy and can severely impact the health of both the mother and the fetus. It’s important to differentiate between HG and morning sickness due to the potential complications associated with the former.
Symptoms of Hyperemesis Gravidarum:
- Severe nausea and vomiting, often more than three times a day.
- A persistent inability to keep food or liquids down.
- Dehydration, indicated by symptoms such as dizziness and a rapid heart rate.
- Weight loss and the presence of ketones in the urine, known as ketonuria.
Causes and Prevalence:
- The exact cause of HG is not fully understood, but it is linked to hormonal changes during pregnancy, specifically the rise in human chorionic gonadotropin (HCG).
- Genetic predispositions may also play a role, with mutations in genes like GDF15 and PGR being associated with HG.
- Studies suggest that HG could affect a larger percentage of pregnancies than previously thought, with some estimates reaching up to 10.8%.
Severity and Duration:
- HG symptoms are significantly more severe than regular pregnancy nausea and vomiting.
- The condition can last for the entire duration of the pregnancy.
- It can lead to dehydration, significant weight loss, and electrolyte imbalances, necessitating medical intervention.
Understanding the severity and potential risks of HG is vital for expecting mothers and healthcare providers to manage pregnancy symptoms effectively and ensure a healthy pregnancy and fetus.
Read : Home Remedies for Morning Sickness: Natural Ways to Find Relief During Pregnancy
Causes and Risk Factors

Hyperemesis gravidarum (HG) is a complex condition with several contributing factors. While morning sickness is a typical pregnancy symptom, HG presents with more severe nausea and vomiting. The causes and risk factors associated with HG are multifaceted and include:
Hormonal Influences:
- A rapid increase in the levels of human chorionic gonadotropin (HCG), a hormone released by the placenta, is considered a primary cause.
- Higher estrogen levels, another hormonal change during pregnancy, are also implicated in HG.
Genetic Predispositions:
- Genetic factors play a role, with a personal or family history of HG increasing the likelihood of occurrence.
- Specific genes, such as GDF15 and IGFBP7, which are related to placental development and appetite regulation, may contribute to the condition.
Risk Factors:
- Previous HG Pregnancy: Women with a history of HG in earlier pregnancies face a higher risk in subsequent ones.
- Multiple Pregnancy: Carrying more than one fetus can increase the risk due to larger placental mass.
- Family History: A first-degree relative with HG suggests a genetic component to susceptibility.
- Other Factors: Younger maternal age, obesity, and a first-time pregnancy are associated with a higher incidence of HG.
Understanding these factors is essential for healthcare providers to identify and manage HG effectively, ensuring the safety and well-being of both the mother and the fetus during pregnancy.
Impact on Health and Pregnancy
Hyperemesis gravidarum (HG), while less common than morning sickness, carries significant risks for both the mother and the developing fetus. The impact of this condition on health and pregnancy outcomes is multi-faceted and requires careful management:
Maternal Complications:
- Nutritional Deficiencies: Inadequate intake due to persistent nausea and vomiting can lead to deficiencies in essential vitamins and minerals.
- Dehydration and Electrolyte Imbalances: Severe vomiting may result in dehydration, leading to electrolyte imbalances which can disrupt normal bodily functions.
- Organ Failure: In extreme cases, the strain on the body from prolonged HG can lead to organ failure.
Fetal Complications:
- Preterm Birth: A meta-analysis has shown a 30% increased risk for preterm birth in pregnancies affected by HG.
- Low Birth Weight: The same analysis reported a 40% increase in risk for low birth weight, a concern that is compounded if the mother experiences significant weight loss during pregnancy.
- Perinatal Outcomes: The risk of small-for-gestational-age (SGA) and perinatal death is also elevated, although some studies suggest that the risk may not be as high once maternal weight gain is adjusted for.
Emotional and Physical Well-being:
- Mental Health: The chronic nature of HG can lead to anxiety, social isolation, and depression, underscoring the importance of psychological support.
- Quality of Life: The persistent and debilitating symptoms can severely impact the daily life and overall quality of life of the expectant mother.
Despite these challenges, with prompt and effective treatment, the risks to the fetus are significantly mitigated. It is, therefore, imperative for those experiencing symptoms beyond typical pregnancy nausea and vomiting to seek medical attention to manage HG effectively.
Managing and Treating Hyperemesis Gravidarum
Managing and treating hyperemesis gravidarum (HG) requires a multi-pronged approach that prioritizes alleviating symptoms, preventing dehydration, and ensuring adequate nutrition for both mother and baby. Following the American College of Obstetrics and Gynecology (ACOG) guidelines, treatment typically begins with non-pharmacologic interventions and may progress to pharmacologic therapy based on the severity of symptoms.
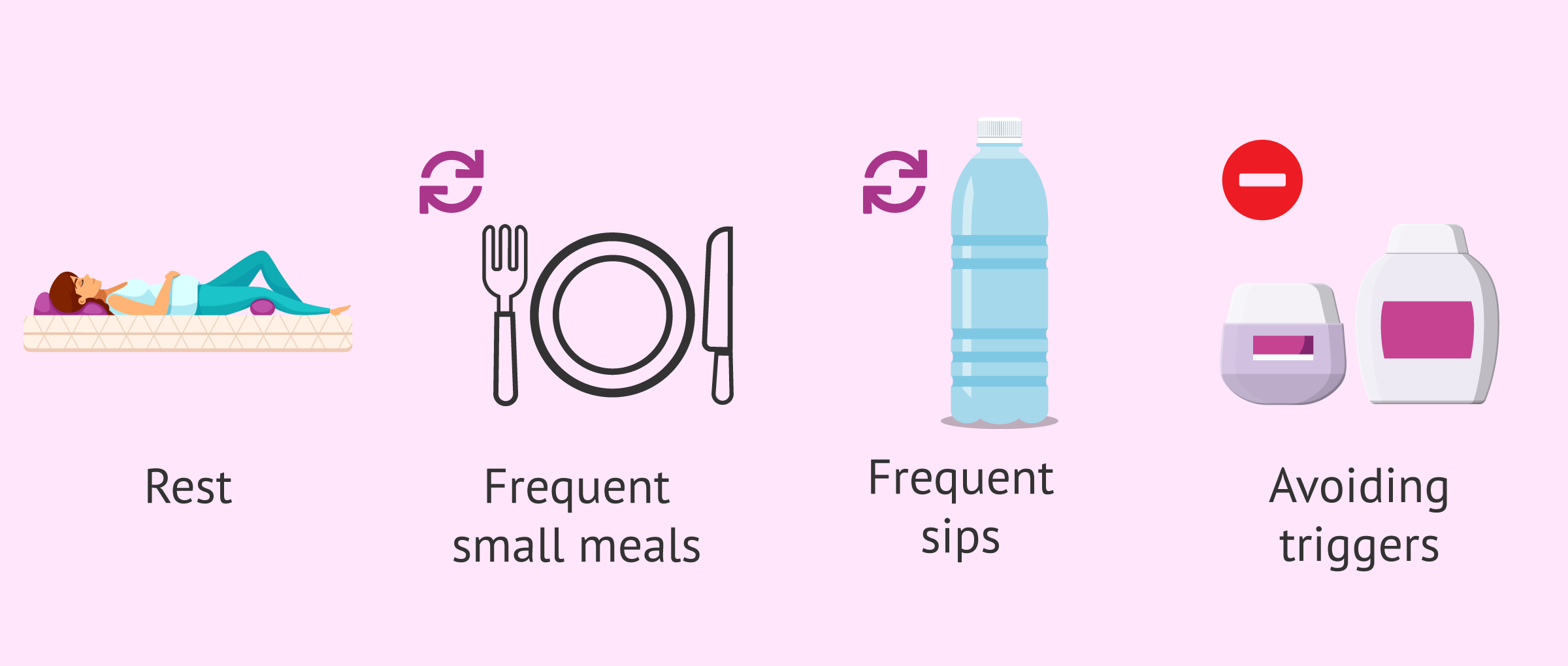
Non-Pharmacologic Interventions:
- Dietary Adjustments:
- Eat smaller, more frequent meals to ease digestion.
- Drink fluids in small amounts throughout the day to maintain hydration.
- Natural Remedies:
- Ginger, known for its anti-nausea properties, may offer relief.
- Vitamin B6 (pyridoxine) and thiamine (Vitamin B1) supplements can help mitigate nausea.
Pharmacologic Therapy:
- First-Line Medications:
- A combination of vitamin B6 and doxylamine is recommended as initial treatment.
- Additional Medications:
- Anti-sickness drugs and antacids to control vomiting.
- IV steroids to reduce inflammation and provide nutrition.
Hospital Treatments for Severe Cases:
- Intravenous (IV) Fluids:
- To treat dehydration and restore electrolyte balance.
- Nutritional Support:
- Tube feeding or total parenteral intravenous nutrition (TPN) may be necessary to ensure the mother and fetus receive essential nutrients.
Complementary treatments like acupressure and hypnosis can be explored under professional guidance. It’s essential to consult healthcare professionals for the appropriate treatment and management of HG, especially since it is considered a high-risk pregnancy condition requiring close monitoring.


